Get paid in 3 weeks!
We process you claims and ensure that you get paid within just 21 days!

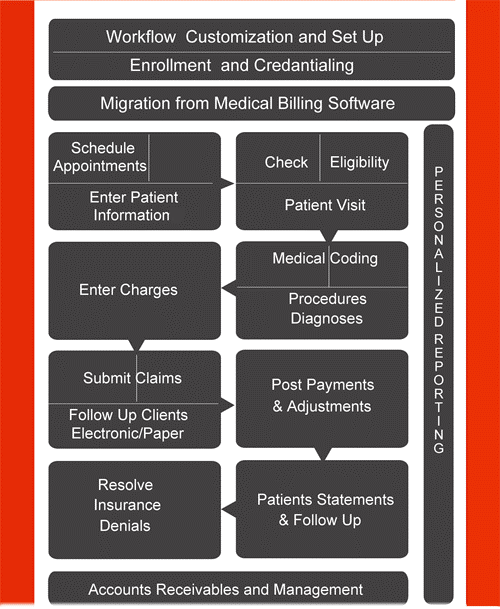
1.We receive provider information through our secure FTP server. We accept superbills, transcripts and any other form of provider documentation for creating claims.
2.Our insurance verification team, check the insurance coverage, patient responsibility, EOB form and demographic details of the patient.
3.Our AAPC certified coding team enters service codes, E/M codes, POS codes, technical codes and modifiers as and when necessary.
4.A thorough claims scrubbing takes place. Our coding manager verifies the accuracy of the coded documents.
5.We create a separate account for each patient and the demographic and insurance details are entered. Appropriate charges for each code is assigned in our charge entry process.
6.We electronically transmit the completed and verified claims to the insurer based on the HIPAA 5010 guideline for transmitting claims.
7.We offer accurate and updated payment posting services.
8.Our 24x7 AR calling team follows up on the claims and lets you know the status of your claims inside of a week.
9.Create secondary claims if necessary, call up patients to collect payment due from them and coordinate with the physician, insurer and patient till the check reaches the table.
10.We have a specialized denial management team to handle denied claims and work on pending AR reports.
With every little aspect covered you can be sure of whittling down your long AR list and collect maximum reimbursement for every claim that reaches the insurer.
We process you claims and ensure that you get paid within just 21 days!
Get the advantage of 24/7 support. Accelerate your billing cycle, now!
Your revenue stream is secure as we have 7 certified teams
Start testing ICD10 and send out claims with our ICD10 specialists