Get paid in 3 weeks!
We process you claims and ensure that you get paid within just 21 days!

Referral requests are important electronic transactions. With healthcare laws closely monitoring referral requests, it is important you maintain a clean record. But how many medical practices spend time on reviewing and analyzing their healthcare transactions ? Unfortunately not many !
The amount of referral requests you might have furnished to insurers, can send you into a tizzy. And to sit through them patiently, and examining the flaws is something you always put off for another day. With the need for pristine documentation in the healthcare industry, nothing can afford to be amiss.
MedicalBillingStar offers to do what you hate doing ! We offer referral request reviewing services as a part of our costless Free Fiscal Fitness Checkup offered for medical practices. Our reports are accurate and exact.
Sleeping at the wheel can deal a fatal blow to your practice. We take absolute control of your documentation requirements and send you a precise report. We follow HIPAA compliant encryption protocols and ensure the data you send us for reviewing is absolutely safe.
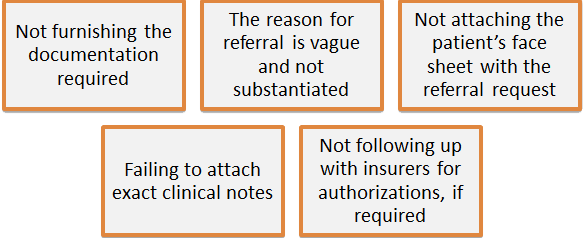
All this takes up lot of time. And ever busy fax machines and phone lines. But, failure to streamline the process, or not tracking metrics, can force you to work, unpaid. MedicalBillingStar can give you the power that exact information can bring to the table.
We track your referral requests, rejection rate, the time it takes for your requests to be processed, and the errors you make. If there is one thing we clearly understand it is the big difference, small changes can make. Perfect documentation forms the crux of a healthy claims revenue cycle. And MedicalBillingStar will help you get closer to your dream of a healthier revenue cycle.
For free claims referral request support call us @ 1 - 877 - 272 - 1572 or fill an inquiry form here.
Fight denied claims right away !

Once a claim is denied, most insurers have a deadline to contest the denial. Our denial management team starts appealing on rejected claims much before that. We act according to the specificities of each insurer, for appealing claims based on the coverage documents and summary of benefits. We revert with the necessary documents required such as a copy of the explanation of benefits, medical records, copies of the denial letter and any other additional documentation that might be required to process claims.
And finally our 24x7 medical billing services can interface with any emr or ehr you use so you can access and keep tabs on your billing 24x7 as well ! Avail our free trial,experience our user friendly medical billing process. We are just a call away. Reach us on our toll-free number @ 1-877 272 1572 or fill out the form here.
We process you claims and ensure that you get paid within just 21 days!
Get the advantage of 24/7 support. Accelerate your billing cycle, now!
Your revenue stream is secure as we have 7 certified teams
Start testing ICD10 and send out claims with our ICD10 specialists