Get paid in 3 weeks!
We process you claims and ensure that you get paid within just 21 days!

Closing your eyes and praying doesn't make rejected claims, go away ! It takes persistent effort to reach your goal of zeroing down denied claims. MedicalBillingStar, as always, helps healthcare providers get a little closer to their goal. Prior authorization requests are important as certain medical treatments or drugs demand authorization.
But most medical practices overlook them. Your busy biller files claims anyway and cannot be bothered to notice the difference between, standardized prior authorization request forms, and insurer specific forms, and guidelines.
To add insult to injury, almost 20% of authorization requests are turned down by insurers. The reason could be an incomplete, incorrect form or, using an NPI that is not on the agency provider file. There are bound to be pitfalls. It is important you note the reason for denial, whether sufficient documentation was submitted and on whether the denied authorization request was followed up on.
MedicalBillingStar offers to let you know whether you are following the prior authorization process right !
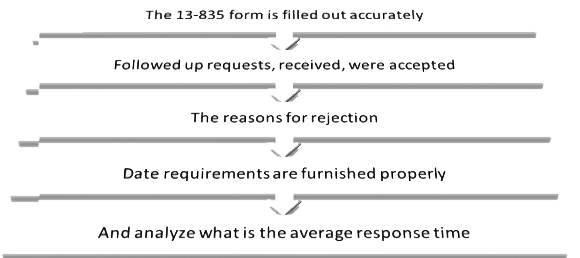
With our through and detailed reports you will identify the flaws in your prior authorization process. And face your insurer armed with facts instead of vague complaints. You will be able to better utilize the time and productivity of your staff.
Our Free Prior Authorization Check i-s a part of our Costless Annual Fiscal Fitness Checkup we offer for medical practices.

Want to get rid of billing worries once and for all ? Work with us and we will take care of your billing and documentation needs. We send out prompt and accurate prior authorization requests to insurers based on the regulations they follow. We also closely follow up on rejected or delayed authorization forms. Our claims revenue cycle experts make sure that both your practice and patients are not the casualties of the cracks in the system !
For free claims authorization request documentation support call us @ 1 - 877 - 272 - 1572 or fill an inquiry form here.
We process you claims and ensure that you get paid within just 21 days!
Get the advantage of 24/7 support. Accelerate your billing cycle, now!
Your revenue stream is secure as we have 7 certified teams
Start testing ICD10 and send out claims with our ICD10 specialists