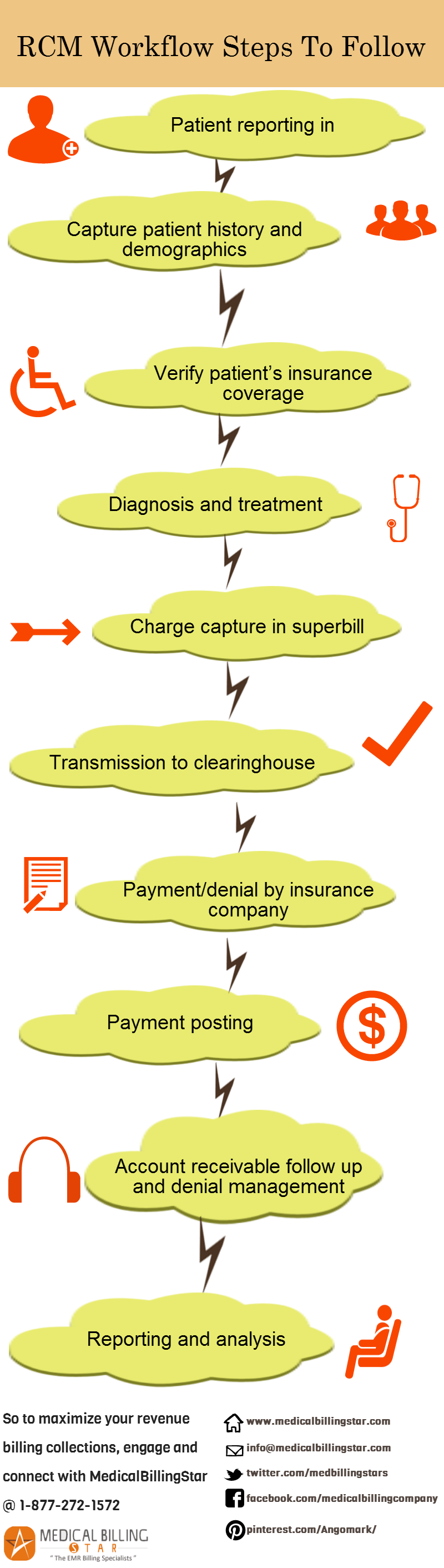
Effective and efficient Revenue Cycle Management (RCM) is bread-and-butter for survival and prosperity of any medical practice business. RCM is not limited to medical billing and collecting reimbursement claims. It involves tightly integrating all the clinical workflow steps, commencing with patient’s registration at the front desk, diagnosis, treatment, discharge, recovery of dues from the patient and the insurance company, and follow up on denied claims.
For ensuring financial viability of the business and before initiating implementation process of RCM, it would be prudent to carry out an in-depth assessment of the current position of the practice.
In-depth Self-examination :
There is a need to evaluate the present standing of the practice with the following posers :
- 1. Does it take unduly a long time to collect reimbursement claims and patient payment?
- 2. Is the denial rate for the first submission of reimbursement rate more than 4%? (For best practice standard the rate should be less than 4%)
- 3. Are write-offs and adjustments of pending reimbursement money very frequent and high?
- 4. Is percentage of accounts receivable, which are more than 120 days old, higher than 10%? (For best practice it should be less than 10%).
If answer to any one of these posers is in the affirmative, then the financial viability of the practice is jeopardized.
Critical Post-evaluation Measures :
Patient Reporting-in :
On receipt of a phone call for an appointment from the patient, the front desk should ascertain medical problem and insurance coverage of the patient, and then guide the patient to provide information for registration by going online on the hospital’s/clinic’s website. Any incomplete information should be followed up before the appointment, so that the insurance coverage of the patient can be verified. An alternative process involves a kiosk for patient check-in at the clinic or hospital for collection of patient’s demographic data and automatic verification of insurance coverage.
Charge Entry and Capture in the Superbill :
As a basic requirement, physicians should ensure that the correct code with appropriate modifier is recorded in the clinical document of the patient, to ensure correct billing and preparation of claims. The billing should be timely and close to the date the patient has been provided with the medical services to avoid delay and piling up of pending claims.
Bill Clearing House :
Bill clearing house checks whether all the required data are included in the bills transmitted to the clearing house by the clinic/hospital.
Follow-up with Insurance Company :
Once the claims are transmitted to the insurance agency, follow-up is a must to ascertain the progress on submitted claims. When the claims are passed, in full or partial, the insurance company remits the payment automatically to the practice account.
Patient’s Portion of Payment :
Ascertain and recover patient’s payment contribution for diagnosis and treatment through aggressive AR callers.
Denied Claims and Follow up :
Correct and resubmit denied claims to the insurance company and follow up till receipt of payment.
Complete End-to-end RCM :
RCM encompasses all the workflow of the clinic or hospital, with each step linked to the next step as under :