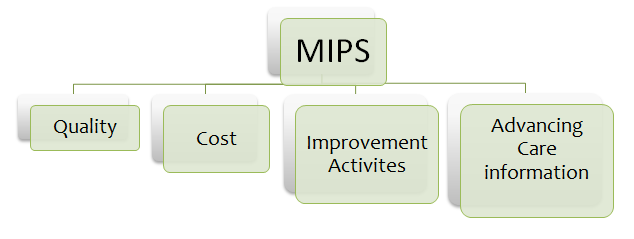
MIPS or Merit-based incentive payment system is one of the two Quality Payment Programs launched by MACRA, the other one being APMs or Alternative Payment models to reward clinicians. MIPS has four connected performance categories that will affect your Medicare payments: Quality, Improvement Activities, Advancing Care Information and Cost. Let me begin by looking at CMS’s current status:

What CMS has been doing to encourage clinicians to participate in these programs?
Handpicked Content:- How to prepare for MIPS in 2018. Download this quick-read PDF to prepare for mips in 2018
- CMS has been observing feedback very closely to make this program a success; i.e. to encourage many new clinicians to participate and the current ones to continue using the program with ease. It’s also trying to finalize proposed policies from 2018 as it will be the final rule with comment period.
- CMS is retaining some of the flexibilities from the transition year to help clinicians prepare for year 3 or 2018
- CMS is offering free technical assistance as an incentive for participation
How to become eligible to participate in MIPS?
- Following already existing quality programs like PQRS, VBPS and MU will make you easily eligible for MIPS
- In order to be eligible for MIPS, you must claim more than $90,000 annually from Medicare or provide care for more than two-hundred patients a year.
- To participate in MIPS you must be one of the following:
- Physicians, which includes doctors of medicine, doctors of osteopathy (including osteopathic practitioners), doctors of dental surgery, doctors of dental medicine, doctors of podiatric medicine, doctors of optometry, and chiropractors; Physician assistants (PAs)
- Nurse practitioners (NPs)
- Clinical nurse specialists
- Certified registered nurse anesthetists
- Any clinician group that includes one of the professionals listed above
Form a multi-disciplinary team
Think of MIPS as a qualifying exam. What matters is that you get a good overall score. It doesn’t matter if you scored more on one subject and less on another. But you want to choose your performance categories that yield maximum output. This is where creating a team that identifies performance categories that work best for your specialty or your practice comes into place. The ultimate goal of implementing MIPS is to get good incentives for your practice forever. Your team should have members from administration, physicians, finance, and operations. Having a multi-disciplinary team will result in good decision making.
Decision Making & Reporting
There are many Quality measures and Improvement activities to choose from. Your multi-disciplinary team should make a combined decision in choosing what measures to report on. T his team should make decisions that are financially lucrative for your organization. There are three ways of reporting: EHR, registry and claims data. Suppose you choose to report through claims data for a particular quality measure but MIPS might have a better benchmark for that same quality measure if it’s done through the registry. As there are 271 quality measures to choose from, physicians have to go through the Quality Payment Program website and figure out which form of reporting will be favorable for them.
his team should make decisions that are financially lucrative for your organization. There are three ways of reporting: EHR, registry and claims data. Suppose you choose to report through claims data for a particular quality measure but MIPS might have a better benchmark for that same quality measure if it’s done through the registry. As there are 271 quality measures to choose from, physicians have to go through the Quality Payment Program website and figure out which form of reporting will be favorable for them.
Changes in 2018
- Solo practitioners or practices with less than ten physicians can form an online virtual team and report MIPS measures together
- CMS will reward five bonus points to clinicians who treat patients with complex mental and physical illnesses.
- CMS is working to reduce the amount of reporting in MIPS to encourage more participation.
- (Beginning 2018)Providers who treat less than 200 patients or fewer Part B Medicare beneficiaries or bill Medicare Part B for $90,000 or less in allowed charges don’t have to report MIPS
- Providers affected by hurricanes don’t have to report MIPS for 2017 and can avoid the penalty in the year 2019. If they wish to submit MIPS data for 2017, they will get payment adjustments and score for the information submitted.
- CMS might assign 10% under cost category in 2018.
Closely follow CMS for changes and /or updates
Closely follow CMS for any changes made to the Quality Payment Program. All updates are published on the CMS.gov website.
 Do you have a successful MIPS Strategy in place? Comment it here and help the physician community perform better.
Do you have a successful MIPS Strategy in place? Comment it here and help the physician community perform better.
Leave a Reply