“We shouldn’t feel sorry for ourselves. A lot of us say, oh my God, how could this be happening. Look at all the unpredictable things happening all the time.These are happening in every industry.”Michael Dowling, CEO of Great Neck
This June didn’t work well for some healthcare systems. Many hospitals struggling financially for years were forced to announce their failure. What could have made these hospitals suffer major revenue losses and file for bankruptcy protection? Let us check the most recent ones who had to face such setbacks and challenges and what you can learn from them.
5 facts I bet you don’t know about Kona Community Hospital!
- The hospital announced that it would be eliminating 34 positions and shutting down its 18-bed skilled nursing service according to KHON
- According to officials, a contingency plan to file a $6 billion budget shortfall which came partly by increased costs of collective bargaining and retiree health benefits resulted in planned cuts and closures.The costs were paid by the state in the past.
- KCH had to face reductions also due to the Hawaii Health Systems Corporation(HHSC) corporate-wide reduction in force and services which was targeted to address a $50 million projected deficit for the entire HHSC system for the FY 2016.
- Employees who lost their positions due to layoffs will be placed in a budgeted vacant position.
- The 18-bed skilled nursing unit could be reopened in the future if required.
-
What made Victory voluntarily file under Chapter 11 of the U.S. Bankruptcy Code?
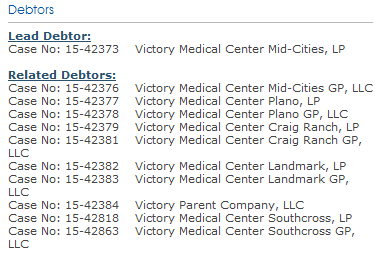
On June 12,2015,the Texas based Victory Healthcare which manages six for profit medical and surgical centers, filed for Chapter 11 of the U.S. Bankruptcy code. Nobilis, a Houston based health system agreed to take over Victory Medical Centre in Plano, Texas for which Victory has reached the court to accelerate the sale. Victory stated it has “many interested buyers for its centers”.
Victory Medical Centre Beaumont and Victory Medical Centre Houston-East are the two centers not included in the filing. These centers don’t need the court process because they have buyers in place.
“We had built an extremely high quality, state-of-the-art group of community-centric medical centers and hospitals,” said Robert N Helms,Jr.,Chairman and CEO and Manager of Victory. “Unfortunately, as out-of-network providers, we came under attack by large insurance carriers. Even though we were able
to execute in-network agreements with three large insurers, the extreme slowness and lack of payment from the carriers constrained liquidity significantly.”
To overcome these challenges, Victory had to cut down on expenses, reduce services but they did not close their emergency rooms.Mr. Helms said, “Unfortunately, now we have no other choice except to sell our facilities with the intent of remunerating secured and unsecured creditors alike.”
Some information about the filing:
Parkview Adventist files for bankruptcy, eyes for merger!
The Brunswick, Maine based medical centre on June 16,2015 filed for Chapter 11 bankruptcy, reported by WCHS6.Randee Reynolds,Parkview President said, “This is not a shock to anyone that’s been here at Parkview. You can only go so far.”
According to officials, the healthcare system, after struggling financially for years, closed its inpatient care and emergency department.Mid Coast Health Services will be getting these 2 services on merger and it will also employ its 180 FTEs.
Brief information about the case filed:
3 lesser known facts about Palomar Health!
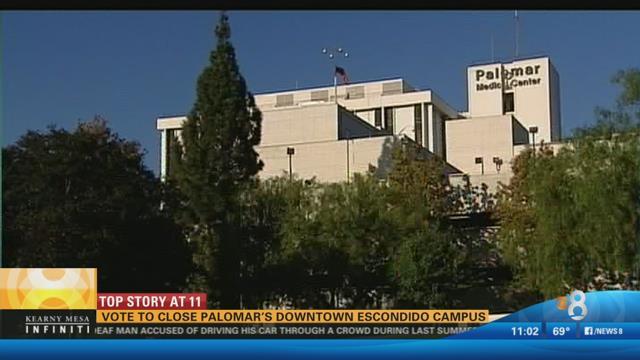
In a 5-2 vote by Hospital directors on June 24, the Escondido, C.A. based Palomar Health Downtown Campus is set to close and shift its existing patient care to sister facilities in 90 days.
- This downtown campus which has 850 people working, houses labor and delivery department, inpatient rehabilitation, behavioral health care, a reserve emergency care and few outpatient surgical services. The Poway based Palomar Medical Center and Pomerado Hospital will be taking over those services.
- Following the patients to the new Poway facilities will be the clinical workers such as nurses and technicians, while those losing their jobs will be support workers. The Palomar’s CEO estimates that between 60 & 75 FTEs and an added 180 to 220 “per diem” part-time workers have to give up their jobs.
- As reported by The San Diego Union-Tribune, due to $20 million operational losses a year and requirement of more than $162 million maintenance costs, the healthcare executives at Palomar recommended closing the downtown medical centre.
What forced Kindred Hospital to target layoffs?
Following the end of Kindred’s lease in Natick by MetroWest Medical Center, the hospital in Boston is aiming layoffs as reported by the Boston Business Journal.
On June 26,2015 the 60 person Kindred hospital, which is part of a larger organization of transitional care and other types of hospitals, closed formally soon after its master the Metrowest put an end to the lease
“We explored several options to move Natick to another location, but determined it was not feasible,” said Amber Hester, Chief Executive Officer at Kindred Healthcare. “We are confident that we will continue to serve the community through our other Kindred hospitals in Boston, Stoughton, and Peabody and our additional lines of service.”
“Almost half of the workers at Natick got jobs at other Kindred centers in M.A.”, Ms, Hester told the, Boston Journal .And her healthcare organization continues to work with employees on finding appropriate jobs.
Kindred is well known for reducing admission rates by 8.4% from 2008-2011.
Why Partners Health decided to cut jobs, closures?
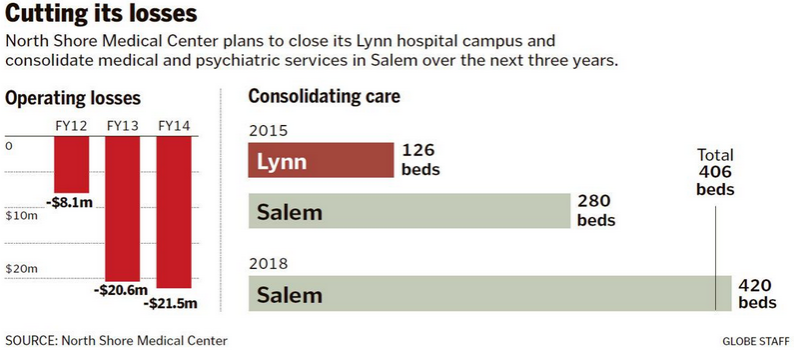
1.In the reestablishment of the NSMC wing of Partners healthcare, all the inpatient services located at Community Hospital will be consolidated at the Salem Campus over the next three years
2.The North Shore Medical Center will rebuild the emergency department, provide,additional 58 beds and 50 new beds for behavioral health.
3.The hospital executives said this plan will target 100 jobs.And they believe to achieve the job cuts through attrition rather than layoffs, according the reports.
4.There’s no date set by the officials for closing the Lynn campus hospital.But the emergency department will be there for over 3 years, and a medical practice with the strength of 16 physicians will stay there.
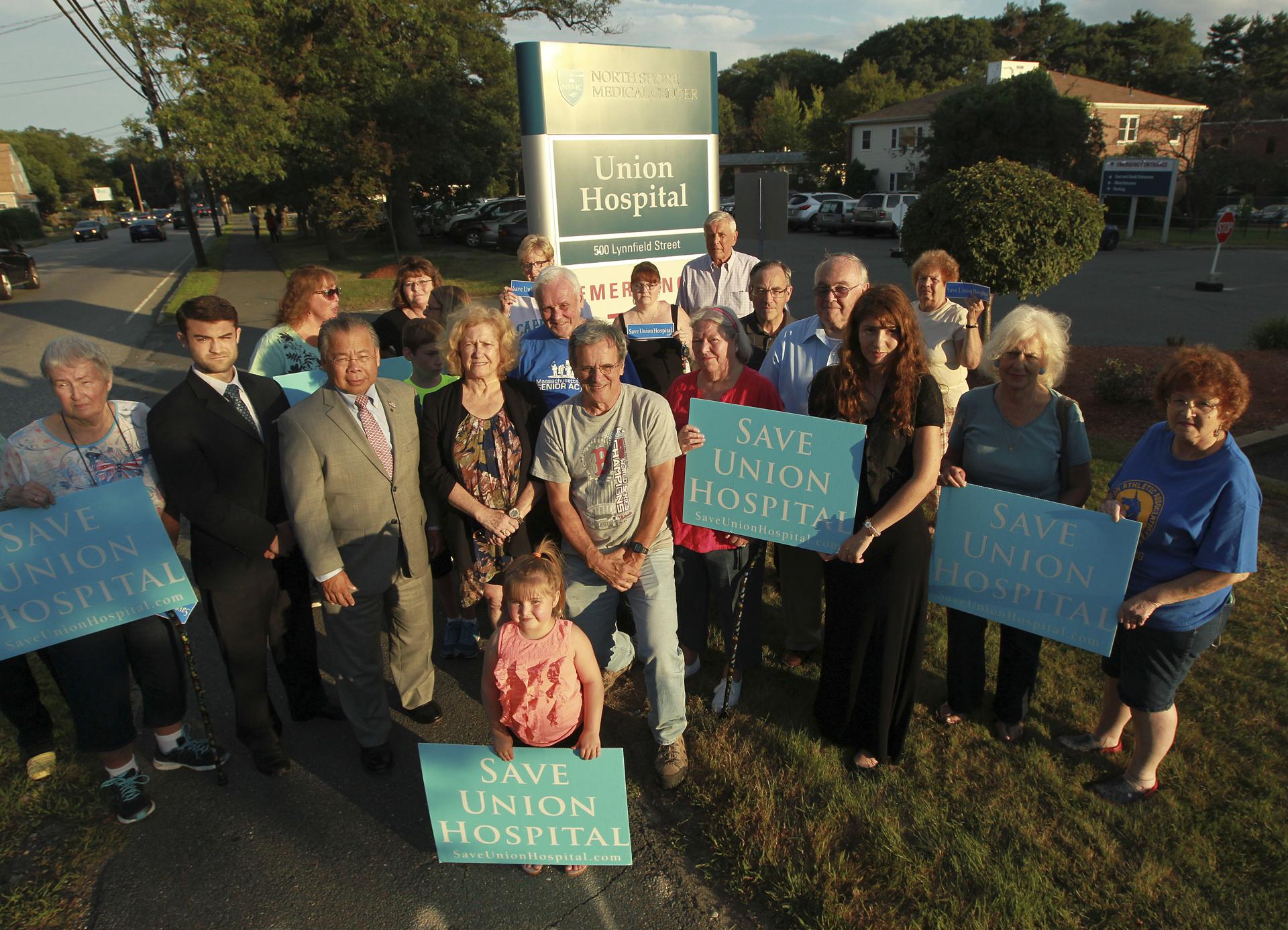
5.Local residents have opposed the decision to close the hospital as they don’t want to see critical medical services shut down. However officials at NSMC believe that this approach would improve patient care at the more advanced and wide ranging Salem campus.
6.The Union hospital was finding it tough to attract patients and thus couldn’t afford to employ specialty care, particularly doctors who specialize in different cardiology types.
7.Due to Medicare and Medicaid insufficient reimbursements both Lynn and Salem lost more than $20 million last year according to Robert G. Norton, president of North Shore Medical Center. Of the patients visiting the Centers, Medicare and Medicaid patients are about 60%.
8.The losses by NSMC over the years were subsidized by Massachusetts General, Brigham and Women’s, the organizations successful wings.
9.One major reason of the medical centers’ plan to close came from,Partners putting their decision on pause, to acquire Hallmark Health Systems.The expected cost savings with the consolidation is to be $18million per year.
Why did Jameson end its Maternity services?
On July 23,2015 New Castle,P.A. based Jamison Hospital announced that it will no longer be providing maternity services with effect from September 1st.
One of the reasons is the uncertainty of the merger of Jamison hospital located in New Castle into the UPMC network. In February the merger was given a formal nod. The officials were expecting the much needed regulatory approvals from Pennsylvania Attorney General, which didn’t happen.
The childbirth services were maintained appreciably well only by two obstetricians for over nine months. It forced the hospital to close its childbirth services when one of the two obstetrician decide to shift her practice to another hospital.
If any OB services arrive after September 1st to the emergency room, the team at Jameson will assess,provide emergency care and transfer appropriately.
The additional staff of childbirth center will be offered to bid on positions available in other wings of the organization.
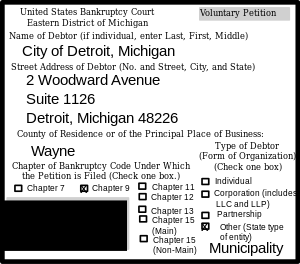
Michigan’s only independent hospital files for bankruptcy!
In their chapter 11 petition filed last month in Detroit, the Pontiac based Doctors Hospital pointed debts between $10 million and $50 million
The doctors hospital was unable to bear the financial losses it received between 2009 to 2013.The physician-owned hospital listed a loss of $11.9 million on net patient revenue of $63.8 million, the latest financial data available, according to the report.
The hospital tried to cut expenses all these years by shutting down its emergency department in October 2013 and targeting 40 layoffs out of the hospital’s 200 employees.But the hospital couldn’t do more to prevent losses and is now under pressure from its investors.
Pro Tips:
What forced these healthcare organizations to file bankruptcy, target layoffs and service closures?
- Attack by large insurance carrier on out-of-network providers
- Struggle to attract patients,
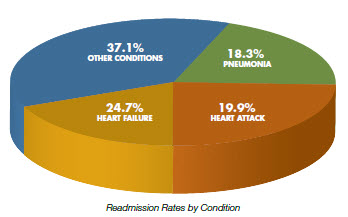
- Low Medicare & Medicaid reimbursements rate
- Uncertainty or failure of a merger.
- Shortage of specialists such as an obstetrician or cardiologist
- Consecutive revenue loss and pressure from investors.
There could be more reasons to force the executives to close a service, file for bankruptcy and target layoffs. When it comes to cutting operational costs, get your employees to identify cost saving opportunities and reward the ones who come with best ideas.
The slow payment process of payers creates a massive revenue backlog. The payers have to implement strategies to improve their payment process.
4 tips from organizations which experienced value of growth from mergers:
- Combine a growth strategy of acquisition and new development.
- Analyzing acquisitions for all the pieces of coordinated care will help you determine the results.
- To form a single system culture compare centralized system leadership with site-based local leadership.
- To fit the organization’s mission, vision and values learn how to identify physician partners and potential hospitals
Healthcare organizations have to take a chance to invest in the expansion of a specialty line. Though the investment is more it will provide valuable care and boost the revenue of the center. Organisations who rely on two or three specialists will be forced towards service closure.
For hospitals that face consistent revenue loss, the best choice would be outsourcing the revenue cycle management to a service with proven expertise.
What actions are you going to take to assure you don’t get listed as one of these hospitals?

Leave a Reply